Table of Contents (click to expand)
Capgras syndrome, first described in 1923, is a syndrome where individuals suffering from it have delusions that their family members have been replaced by identical-looking clones.
What would happen if familiar things suddenly took on a strange form?
In 1923, almost a century ago, French psychiatrist Joseph Capgras described a peculiar case of a Mademoiselle M. She claimed that imposters who looked exactly like her family members had replaced them and planned to harm her. She was also convinced that she was substituted at birth and was in fact an heiress to a great fortune and not really herself.

Joseph Capgras called this “L’illusion des sosies” or “the illusion of look-alikes”, today known as Capgras Syndrome. Capgras’s patients suffered from a set of delusions that were later grouped under the banner of Delusional Misidentification Syndromes or DMS.
What Are Delusions?
A person is said to have delusions when they hold a clearly false belief with utmost conviction, regardless of the evidence available against it. They are completely convinced that their false belief is, in fact, a part of reality.
A few delusions included under DMS are:
- The delusion that your relatives or close ones have been replaced by a “double” or an “imposter” who looks exactly like them is known as Capgras delusion.
- The belief that you have been substituted by someone else is known as Intermetamorphosis.
- Another delusion involves patients thinking that several people they encounter in their life are actually the same person disguised as multiple persons. This is known as the Fregoli Syndrome.
- Yet another delusion, known as the Cotard delusion, convinces patients that they are not really alive, but rather dead or rotting.

All these delusions are also known as persecutory delusions, wherein people cannot distinguish between reality and their false beliefs.
Capgras delusion is the most frequent of the DMSs. Even so, it is very rare. In a study done by a psychiatric hospital in Turkey, only 1.3% of 920 patients admitted over five years suffered from this delusion.
Capgras syndrome does not happen in isolation. It might be a symptom of a broader mental illness, such as schizophrenia spectrum disorders, schizoaffective disorders, and bipolar affective disorders.
Capgras delusion is also seen in patients suffering from neurological problems, such as strokes, brain tumors, epilepsy, and dementia.
Also Read: Why Do Intelligent People Constantly Doubt Themselves?
The Neuroscience Behind Capgras Syndrome
In his original paper, Capgras mentioned that his patient had no trouble remembering the faces of those who were close to her, like her daughter and her husband, whom she believed to have been replaced by imposters. It was, however, the component of familiarity that seemed to have been lost. Mademoiselle M. could no longer form a link of familiarity between the known faces of her family.
Capgras’s observations would end up being more or less in line with the results of brain studies done later on in patients suffering from this delusion.
Whether a face is familiar to us or not can be detected by our emotional response to that face, which can, in turn, be calculated by a method known as Skin Conductance Response.
Our palms are dotted with sweat glands that can make them feel clammy, especially when we’re nervous, like before giving a class presentation. But why do the sweat glands in our palms activate when we feel nervous? This is because of the sympathetic nervous system (SNS), which activates them during “fight-or-flight” situations to cool down our body.
As the “fight-or-flight” response is an emotional reaction to fear that increases our sweat production, our emotional reaction to known faces is also controlled by the SNS, which activates the sweat glands on our palms.

The Skin Conductance Response is measured by attaching electrodes to our palms that conduct a small, constant voltage. When our palms sweat due to emotional arousal, changes in the voltage (if you can recall, salt water increases conductance) can be detected. These changes are directly proportional to our emotional reactions.
Although the mechanisms behind Capgras delusions are not fully known, theories point towards dysfunction in the brain areas responsible for the functions that are compromised in patients with Capgras syndrome:
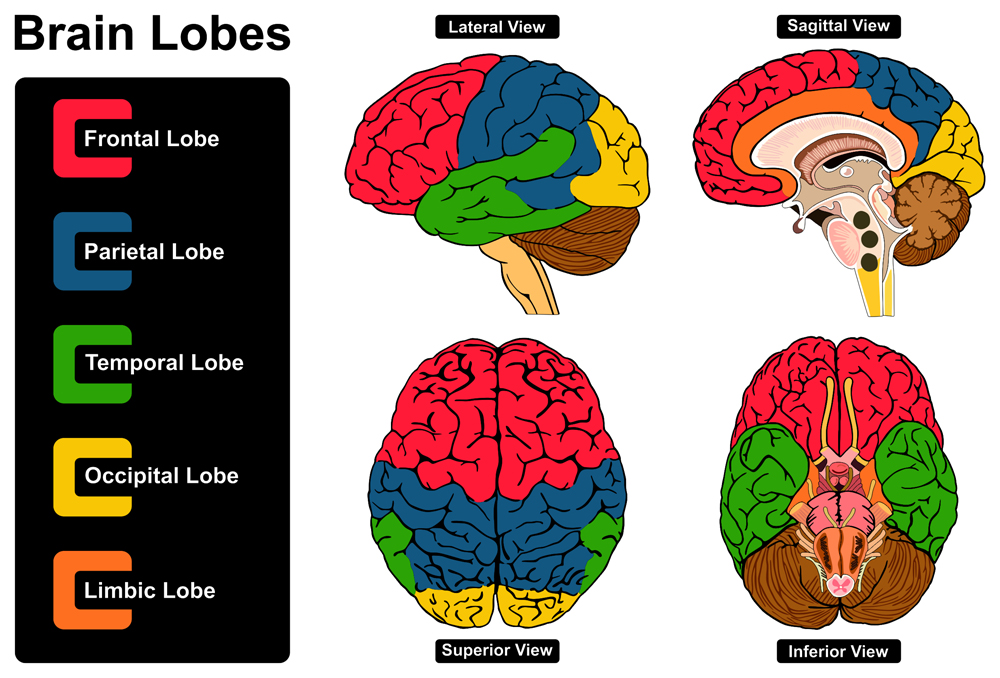
- Since the patients cannot find an emotional connection to the faces of their relatives, a disconnect has been suggested between the temporal lobe of the brain (involved in processing information related to faces) and the limbic system of the brain (involved in processing emotions).
- Delusions have also been strongly correlated to a lack of executive function that is observed in patients suffering from neuropsychiatric illnesses. People with executive dysfunction struggle to carry out normal tasks, such as planning, managing their time, solving problems, and even correcting wrong beliefs when presented with evidence. All these activities are associated with the frontal lobe of the brain. Therefore, this hypothesis suggests a disconnection between the frontal lobe and other regions of the brain, a disconnect that makes the patients unable to correct their delusions.
Also Read: Déjà Vu: Why Do You Get That ‘This Has Happened Before’ Feeling?
Conclusion
Capgras and other delusions highlight the peculiar way that our brain works. The loss of connection between different brain regions brought on by neuropsychiatric problems can cause us to think that our parents have been replaced by an imposter who looks exactly like them or even that we’re no longer a living person—but a corpse!
This also calls into question what we might be able to experience if we could form new connections or reroute our brain wirings, as happens during neuroplastic changes. Could we perhaps be able to experience an entirely new reality?
There is no cure for the delusions that manifest in Capgras Syndrome, but medications that treat the neurological or psychiatric illnesses causing these delusions can bring relief to patients.
How well do you understand the article above!

References (click to expand)
- (2022) Capgras Syndrome - StatPearls - NCBI Bookshelf. National Center for Biotechnology Information
- (2017) She's Not My Mother: A 24-Year-Old Man With Capgras .... The National Center for Biotechnology Information
- Pandis, C., Agrawal, N., & Poole, N. (2019). Capgras’ Delusion: A Systematic Review of 255 Published Cases. Psychopathology. S. Karger AG.
- Chaudhury, S., & Kiran, C. (2009). Understanding delusions. Industrial Psychiatry Journal. Medknow.
- Laine, C. M., Spitler, K. M., Mosher, C. P., & Gothard, K. M. (2009, April). Behavioral Triggers of Skin Conductance Responses and Their Neural Correlates in the Primate Amygdala. Journal of Neurophysiology. American Physiological Society.
